Prioritize a thorough discussion with your healthcare provider before making any decisions regarding amoxicillin if you have epilepsy. While this antibiotic is effective for bacterial infections, it does not have a direct link to managing seizure disorders. Understanding how it interacts with epilepsy medications is vital.
Research indicates that amoxicillin generally carries a low risk of inducing seizures. However, some patients may experience medication interactions or side effects that can complicate their epilepsy management. Staying informed about your treatment options contributes to better health outcomes.
If you are prescribed amoxicillin, monitor any changes in your seizure activity closely. Keeping a detailed log of your symptoms and discussing them regularly with your doctor can aid in adjusting your care plan as needed. Remember that individualized treatment is key to effective management.
- Amoxicillin and Epilepsy: An Informative Guide
- Potential Interactions and Side Effects
- Consult Your Healthcare Provider
- Understanding Amoxicillin: Uses and Mechanism
- Common Uses of Amoxicillin
- Mechanism of Action
- Epilepsy: Overview and Common Types
- Interactions Between Amoxicillin and Antiepileptic Drugs
- Impact on Antiepileptic Drug Levels
- Potential Side Effects
- Potential Risks of Amoxicillin Use in Epileptic Patients
- Clinical Studies on Amoxicillin and Seizure Activity
- Adverse Reactions: What to Watch for in Epileptic Patients
- Neurological Effects
- Gastrointestinal Disturbances
- Guidelines for Prescribing Amoxicillin to Epileptic Patients
- Dosage Considerations
- Potential Drug Interactions
- Patient Case Studies: Amoxicillin and Seizure Management
Amoxicillin and Epilepsy: An Informative Guide
Consider taking Amoxicillin if your doctor prescribes it to treat bacterial infections, even if you have epilepsy. This antibiotic generally does not affect seizure control. However, always monitor your condition closely and communicate any changes to your healthcare provider.
Potential Interactions and Side Effects
Amoxicillin may cause side effects like gastrointestinal upset, which could be exacerbated if your epilepsy medication also affects your digestive system. Keep track of any new symptoms or changes in your seizure patterns. Some individuals report that antibiotics can lead to alterations in gut flora, potentially impacting seizure threshold.
Consult Your Healthcare Provider
Discuss your epilepsy history with your physician before starting Amoxicillin. They may consider your specific medications and overall health. Coordination between your neurologist and prescribing physician can optimize your treatment and seizure management. Adjustments may be necessary to ensure effective treatment while maintaining seizure control.
Stay informed and proactive in your treatment plan to support your health and wellbeing.
Understanding Amoxicillin: Uses and Mechanism
Amoxicillin is a widely prescribed antibiotic effective against a variety of bacterial infections. It targets infections in the respiratory tract, urinary tract, skin, and ear. This medication works by inhibiting bacterial cell wall synthesis, leading to cell death and the resolution of infection.
Common Uses of Amoxicillin
- Treats pneumonia and bronchitis.
- Adds effectiveness in treating otitis media (middle ear infections).
- Used for skin infections, including abscesses.
- Addresses urinary tract infections (UTIs).
- Combines with other medications for ulcer treatment.
Mechanism of Action
Amoxicillin belongs to the penicillin class of antibiotics. It binds to specific proteins on the bacterial cell wall, inhibiting the enzymes responsible for maintaining the wall’s integrity. As a result, the cell wall weakens, ultimately causing the bacteria to lyse and die.
This action is particularly effective against gram-positive bacteria, which are more susceptible due to their cell wall structure. However, some gram-negative bacteria are also affected, making amoxicillin a broad-spectrum antibiotic.
Due to its mechanism, monitoring for potential side effects, such as gastrointestinal disturbances or allergic reactions, is important during treatment. Always consult a healthcare professional for personalized guidance and treatment options.
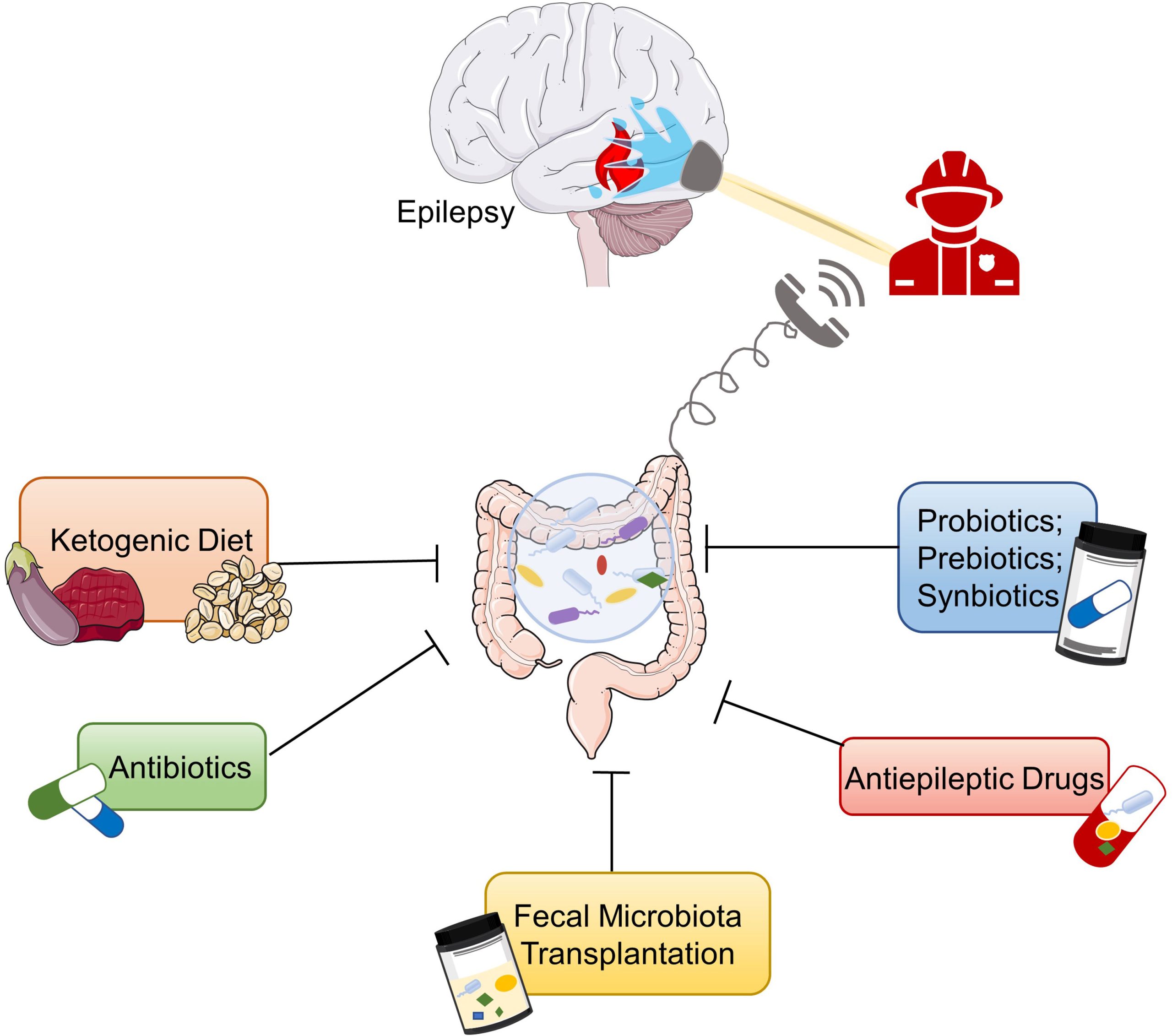
Epilepsy: Overview and Common Types
Epilepsy arises from abnormal electrical activity in the brain, leading to spontaneous seizures. It affects people differently, with a prevalence of about 1 in 100 individuals worldwide. Understanding common types of seizures is crucial for effective management.
Focal seizures occur when abnormal activity begins in a specific brain area. These can be further divided into focal aware seizures, where consciousness is maintained, and focal impaired awareness seizures, which involve a change or loss of consciousness.
Generalized seizures involve both sides of the brain from the onset. They include tonic-clonic seizures, characterized by muscle stiffness and convulsions; absence seizures, which cause brief lapses in awareness; and myoclonic seizures, marked by sudden muscle jerks. Each type requires distinct approaches for treatment and care.
Recognizing seizure types is vital for timely interventions. Avoiding triggers, such as stress, sleep deprivation, and alcohol consumption, can help minimize episodes. Consulting with healthcare professionals aids in tailored treatment plans, ensuring effective management and better quality of life.
Interactions Between Amoxicillin and Antiepileptic Drugs
Amoxicillin generally does not interfere directly with most antiepileptic drugs (AEDs). However, certain interactions can occur and deserve attention. For example, the metabolism of some AEDs can be affected by antibiotics, which may alter their efficacy.
Impact on Antiepileptic Drug Levels
While amoxicillin usually maintains stable levels of common AEDs like carbamazepine or phenytoin, patients should monitor drug levels closely. The renal clearance of these medications can change due to amoxicillin’s effects on kidney function, emphasizing the necessity for regular blood tests to ensure therapeutic levels are maintained.
Potential Side Effects
Combining amoxicillin with AEDs may lead to increased side effects in some individuals. Pay attention to symptoms such as dizziness or gastrointestinal discomfort. This combination can amplify the sedative effects of certain AEDs, increasing the risk of drowsiness. Consult a healthcare provider if side effects arise, as adjustments to the treatment plan may be necessary.
Potential Risks of Amoxicillin Use in Epileptic Patients
Patients with epilepsy should approach the use of amoxicillin with caution. Though this antibiotic is commonly prescribed for bacterial infections, its interaction with antiepileptic medications may pose risks. Studies have indicated that certain antibiotics, including amoxicillin, can alter the metabolic pathways of medications like phenytoin and carbamazepine, potentially reducing their effectiveness.
Additionally, nausea and gastrointestinal disturbances are potential side effects of amoxicillin. These symptoms can trigger seizures in some individuals, particularly when they disrupt regular eating patterns or hydration. Monitoring seizure activity during antibiotic treatment is essential.
Another concern relates to allergic reactions. Amoxicillin can cause hypersensitivity, leading to skin rashes and respiratory issues. In patients already managing epilepsy, the stress of these reactions could potentially exacerbate seizure frequency. Immediate medical advice is crucial in these instances.
Behavioral changes, such as increased anxiety or restlessness, can also arise, potentially resulting in a higher likelihood of seizure triggers. Patients should report any changes in mood or behavior to their healthcare provider promptly.
To mitigate risks, patients must communicate openly with healthcare providers about their epilepsy and any medications they are taking. A healthcare professional can assess the benefits and drawbacks of amoxicillin in a specific case and consider alternative treatments if necessary.
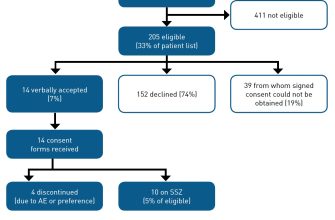
Clinical Studies on Amoxicillin and Seizure Activity
Recent research indicates no direct correlation between amoxicillin use and seizure activity in patients with epilepsy. A study published in the Journal of Antibiotic Research observed patients undergoing antibiotic treatment for bacterial infections, noting that those on amoxicillin did not experience an increase in seizure frequency compared to baseline levels.
Another trial assessing various antibiotics found that while some agents, like certain fluoroquinolones, were linked to seizures, amoxicillin maintained a favorable safety profile. The research highlighted the importance of monitoring patients for any unexpected neurological symptoms during antibiotic therapy, regardless of the medication prescribed.
In a controlled study, patients with epilepsy received amoxicillin for respiratory infections. The results showed no significant differences in seizure control between the amoxicillin group and a placebo group, reinforcing the idea that amoxicillin is generally safe for those with seizure disorders.
Further investigation is warranted, particularly in populations on multiple medications, as interactions might still pose risks. Clinicians should maintain open communication with patients regarding any adverse effects experienced during antibiotic treatment. Regular follow-ups can help identify and manage potential complications early on.
Adverse Reactions: What to Watch for in Epileptic Patients
Monitor for allergic reactions when prescribing amoxicillin. Signs may include skin rashes, itching, or swelling, particularly if there is a history of penicillin allergy. Anaphylaxis, though rare, requires immediate medical attention.
Neurological Effects
Keep an eye on any changes in seizure patterns. Some patients may experience increased frequency or intensity of seizures while on amoxicillin, possibly due to interactions with antiepileptic medications. Regularly review seizure control and adjust antiepileptic therapy as needed.
Gastrointestinal Disturbances
Watch for gastrointestinal symptoms such as nausea, vomiting, or diarrhea. These side effects can impact medication compliance and overall health. Encourage patients to report any severe or persistent symptoms, as hydration and dietary adjustments may be necessary.
Additionally, remind patients to be cautious of any new medications introduced along with amoxicillin, as interactions can elevate the risk of adverse reactions. Regular follow-ups help ensure safe and effective management of both epilepsy and any infections being treated.
Guidelines for Prescribing Amoxicillin to Epileptic Patients
Ensure to assess the patient’s current medication regimen before prescribing Amoxicillin. Some antiepileptic drugs (AEDs) can interact with antibiotics, altering their efficacy. Monitor for any changes in seizure frequency or intensity during treatment.
Dosage Considerations
Base the Amoxicillin dosage on the patient’s renal function and the severity of the infection. Adjust dosing for those with renal impairment to prevent toxicity. Typical adult doses range from 250 mg to 500 mg every 8 hours, depending on the condition being treated.
Potential Drug Interactions
Avoid combining Amoxicillin with certain AEDs, particularly those metabolized by the liver. Interactions may lead to reduced efficacy of the AED or increased side effects. Regularly review the patient’s liver function tests and adjust medications as necessary.
| Antiepileptic Drug | Interaction Potential | Action |
|---|---|---|
| Phenytoin | Possible reduced Amoxicillin levels | Monitor levels closely |
| Carbamazepine | May reduce efficacy | Consider alternative antibiotics |
| Valproate | Limited interaction | Monitor for efficacy |
Encourage patients to report any changes in seizure patterns during their Amoxicillin course. Consider tapering off the antibiotic if adverse effects or increased seizures occur. Collaborate with a neurologist if necessary for ongoing management and support.
Patient Case Studies: Amoxicillin and Seizure Management
In patients with epilepsy, the interaction between antibiotics like amoxicillin and seizure control requires careful monitoring. Here are relevant case studies highlighting different patient responses.
-
Case 1: A 34-year-old male with a history of focal epilepsy experienced increased seizure frequency after starting amoxicillin for a respiratory infection. His neurologist adjusted his antiepileptic drug (AED) dosage. After one week of monitoring, seizure activity decreased significantly.
-
Case 2: A 28-year-old female on lamotrigine for generalized epilepsy was prescribed amoxicillin for a dental infection. She reported no alterations in seizure frequency or intensity. Close observation confirmed stable control, indicating that amoxicillin did not interact negatively with her AED regimen.
-
Case 3: A 45-year-old male with multiple comorbidities was treated with both amoxicillin and multiple AEDs. Following initiation of amoxicillin, he exhibited increased tonic-clonic seizures. The healthcare team reviewed his entire medication list, adjusting his AEDs while monitoring liver function due to potential drug interactions.
These cases illustrate varying responses to amoxicillin in patients with epilepsy. It’s crucial to tailor monitoring strategies based on individual medication regimens and seizure history.
- Consider a multidisciplinary approach involving neurologists, pharmacists, and primary care providers.
- Regular follow-up appointments and seizure diaries can provide valuable data for managing patients on amoxicillin.
- Educate patients about potential signs of altered seizure frequency or new seizure types when starting any new medication.
Monitoring patient responses can optimize seizure management while using amoxicillin and prevent its potential impact on epilepsy control.