Maintain strict hold parameters for Cardizem to ensure patient safety and optimal therapeutic outcomes. Monitor vital signs closely before and after administration. If the heart rate is below 60 beats per minute or blood pressure drops significantly, consider withholding the dose.
Regularly assess the patient’s response to Cardizem therapy. If signs of hypotension, dizziness, or bradycardia appear, reassess the hold criteria. Timing of drug administration can affect responses; therefore, always document any adjustments made to the schedule.
Ensure that healthcare providers are well-informed about the hold criteria specific to Cardizem. Education regarding identification of adverse effects enhances patient safety. By adhering to these guidelines, you effectively manage potential risks while optimizing the benefits of Cardizem treatment.
Cardizem Hold Parameters: A Practical Guide
Hold Cardizem if the patient’s heart rate falls below 50 beats per minute. Maintaining a minimum heart rate is crucial to prevent bradycardia symptoms, which could include dizziness and fainting.
Blood Pressure Monitoring
Monitor blood pressure closely. Hold Cardizem if systolic blood pressure drops below 90 mmHg. Hypotension poses serious risks, and adjusting the dosage or holding the medication may be required to stabilize the patient.
Electrolyte Levels
Check potassium levels periodically. If hyperkalemia occurs, consider holding Cardizem as elevated potassium can increase the risk of life-threatening arrhythmias. Evaluate renal function as well, since impaired kidney function can affect drug clearance.
Understanding Cardizem: Mechanism of Action and Indications
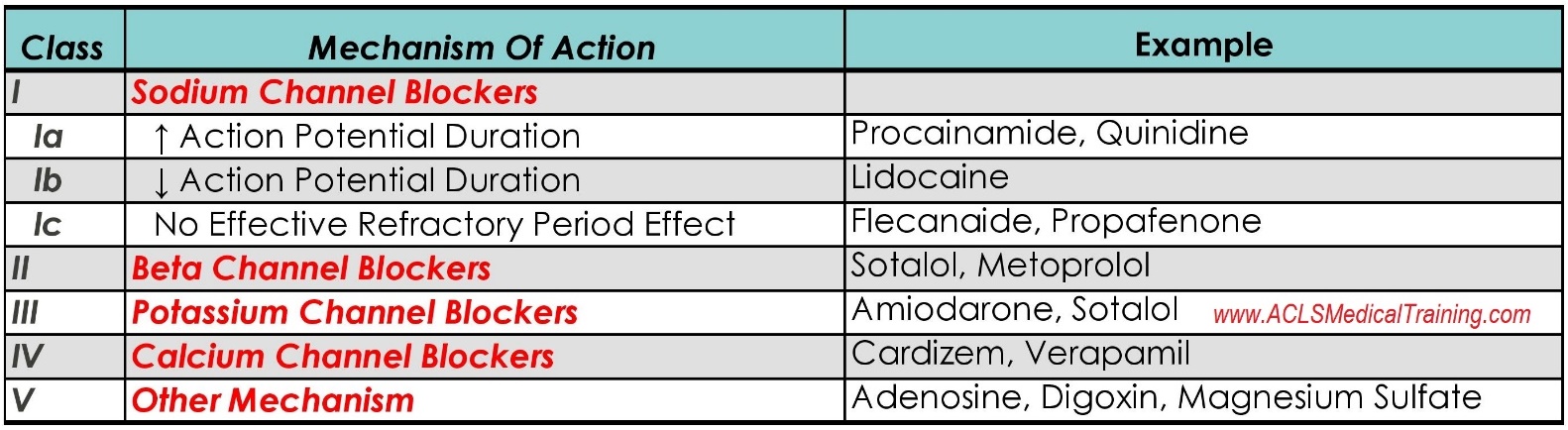
Cardizem primarily acts as a calcium channel blocker, specifically targeting the L-type calcium channels in the heart and blood vessels. By inhibiting these channels, it decreases intracellular calcium levels, resulting in relaxation of vascular smooth muscle. This process leads to vasodilation, ultimately reducing blood pressure and improving myocardial oxygen delivery.
This medication finds its indications in treating various cardiovascular conditions. It effectively manages hypertension, alleviates angina pectoris, and is utilized in controlling certain types of supraventricular tachycardia. Cardizem’s ability to lower heart rate makes it especially beneficial for patients with atrial fibrillation or flutter.
In terms of administration, Cardizem can be given orally or intravenously depending on the clinical scenario. Dosage varies based on the patient’s condition and response to treatment, highlighting the importance of regular monitoring to achieve optimal outcomes.
Potential side effects include dizziness, peripheral edema, and low heart rate, necessitating careful observation during therapy. Patients should be educated on signs of adverse reactions to ensure timely assistance if issues arise.
Overall, Cardizem serves as a valuable tool in the management of specific cardiovascular diseases, providing both symptom relief and improved quality of life for many patients.
Clinical Considerations for Holding Cardizem: Key Patient Assessments
Assess heart rate and rhythm before administering Cardizem. Hold the medication if the heart rate is below 60 bpm or if there are signs of significant bradycardia.
Monitor blood pressure regularly. If systolic blood pressure falls below 90 mmHg, delay the dose.
Evaluate for signs of heart block. If patients exhibit second- or third-degree heart block without a functioning pacemaker, withhold Cardizem.
Assess renal function by checking creatinine levels. In patients with significant renal impairment, consider holding Cardizem to prevent drug accumulation.
Observe for symptoms of heart failure, including dyspnea, edema, or significant weight gain. In such cases, holding Cardizem may be necessary.
Review concurrent medications. Identify any drugs that may interact adversely with Cardizem and consider adjusting the regimen accordingly.
- Be cautious in patients with hepatic impairment. Adjust dosing or hold medication based on liver function tests.
- In patients with a history of hypersensitivity or severe adverse reactions to calcium channel blockers, avoid administration.
- Monitor for signs of hypotension or severe dizziness during initial treatment phases.
Communicate with the healthcare team regarding any concerns or changes in patient status. Collaboration ensures optimal patient care and promotes safety.
Patient Management Strategies: Protocols for Cardizem Hold Situations
When experiencing a significant drop in heart rate or blood pressure, immediately reassess the necessity of Cardizem. Hold the medication if the heart rate falls below 60 beats per minute or if systolic blood pressure drops below 90 mmHg. Notify the healthcare provider promptly to determine the best course of action.
Monitor vital signs closely after holding Cardizem. Check heart rate and blood pressure every 15 minutes until stabilization occurs. Document all findings clearly in the patient’s chart, including changes that occur after the hold.
Review the patient’s medical history for any signs of bradycardia or hypotension. Collaborate with the healthcare team to evaluate possible alternative therapies or adjustments to the current regimen. Engage in discussions about the patient’s cardiac status, potential interactions, and any recent changes in their condition.
Educate the patient on signs and symptoms to monitor, including dizziness, lightheadedness, or worsening chest pain. Encourage them to report any of these immediately. Establish a follow-up plan to revisit the decision to hold Cardizem, considering factors like patient tolerance and overall health improvement.
Evaluate the need for additional medications to manage symptoms during the hold period. Adjust diuretics or beta-blockers as needed, based on the patient’s current status and healthcare provider recommendations. Utilize patient-centered interventions, ensuring they understand the reasons for changes in medication administration.
Consider using non-pharmacological interventions, such as fluid management or lifestyle modifications, to support cardiac health during this time. Encourage activities that promote relaxation and stress reduction, as these can have a positive impact on heart rate control.
Reassess the patient’s condition continually. As the clinical picture evolves, make necessary adjustments to the treatment plan. Foster open communication between the healthcare team and the patient to ensure clarity and support.